Overview
Euthanasia is “an act or omission which, of itself and by intention, causes death, usually in order to eliminate suffering, (perceived or real)”. This term often encompasses the similar practice of physician- assisted suicide, in which a person enlists the aid of others to set-up the means for them to end their own life. These acts generally involve the terminally ill, people with disabilities, older people and people living with chronic pain.
The word “euthanasia” derives from a Greek word meaning “good death” and is sometimes also known as “mercy killing”. The debate is generally seen as an ethical confrontation between Judeo-Christianity and Humanist groups, and it is now a topic being fought out in the political arenas.
Common forms of euthanasia involve the administration of lethal injections or the negligent withholding of vital human necessities in order to cause death, such as food, water and essential medications.
Common arguments made in Support of Euthanasia
- Freedom of choice argument – this should include the right to control one’s own body and life. Furthermore, the state should not be allowed to create laws that prevent people being able to choose when and how they die.
- The pragmatic argument – euthanasia is allegedly already a widespread practice, hence it is better to regulate it.
- The rational argument – if a person has decided on rational grounds that their life has lost its meaning, then they should be permitted to end their life, and this decision should be respected.
- The humanist argument – humanists argue that it is not a moral act to postpone the inevitable, with no foreseeable intervening benefit.

Why Euthanasia Is Not the Answer
Whether it is despair, guilt at being “a burden” upon others, or even the result of a carer who no longer sees value in the fulfilment of their role, euthanasia is the action of a person who has given up. Our role is to support people. Older people and people with disabilities can be especially vulnerable to thinking that they have no worth and this can be overwhelming. The support of loved ones, neighbours and others in the community can demonstrate the dignity of the individual, and their potential to contribute to the happiness of those around them.
The appropriate approach to assisting the vulnerable is through patience and care. Much recognition is due to the dedicated carers who use their lives to improve the quality of the lives of others. Carers can help a person see their own value and dignity. In the instances where a patient is suffering from a terminal condition accompanied by debilitating pain or other symptoms, palliative care offers the hope of a meaningful improvement or resolution of symptoms in a supportive environment.
Palliative Care
The objective of palliative care is to ensure the best possible quality of life for the patient. Palliative care provides the following:
- affirms life and treats dying as a normal process.
- neither hastens nor postpones death.
- provides relief from pain and other distressing symptoms.
- integrates the physical, psychological, social, emotional and spiritual aspects of care, with coordinated assessment and management of each person’s needs.
- offers a support system to help people live as actively as possible until death; and
- offers a support system to help the family cope during the person’s illness and in their own bereavement.
Video
Dr. John Obeid presentation
Euthanasia – Impacts on the Healthcare of the Elderly
2012 Life & Family conference
Mr. Michael McAuley presentation
Euthanasia – The Perspective of John Finnis
2012 Life & Family conference
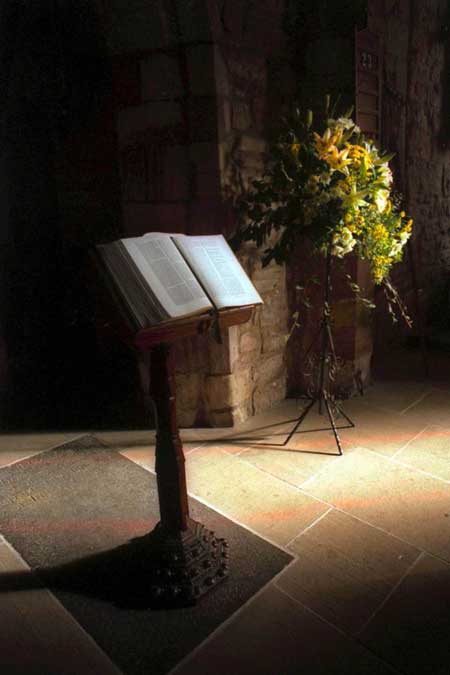
Church teaching on Euthanasia
The Catholic Church clearly teaches that all forms of euthanasia are wrong. The key principle is that one does not will to cause death. The Church founds its teachings in the dignity of humankind, recognising human life as a gift from God. In its Declaration on Euthanasia (1980), the Sacred Congregation for the Doctrine of Faith noted that to end one’s life is to reject God’s love for us.
The Church acknowledges that psychological changes caused by the experience of prolonged suffering may lessen, or even eliminate, the culpability of one who seeks for themself euthanasia, but stresses again and again that the act of euthanasia is always wrong.
On the question of the suffering of a patient, the Church encourages us to consider uniting our sufferings with those of Christ, in union with the redeeming sacrifice which He offered in obedience to the Father’s Will. Nevertheless, the Church is quite clear in permitting palliative care and the administering of pain medication, and encourages this as good and proper.
Finally, the Church teaches that a patient has a right to refuse certain treatments that would merely prolong life with no hope of improvement, but high likelihood of additional pain or risk to the patient’s situation. An example of this would be refusing to undergo an experimental operation that could possibly add three months to your life expectancy, but was considered a risky operation that may cause pain or unacceptably long hospitalisation, thus reducing the time and opportunity a dying person has to spend with their family or being engaged in their community. This concession does not include the withholding of food from a patient, declaring that basic human needs such as food and water, must be supplied to the patient (unless its provision is unjustifiably burdensome or puts the dying person at risk).
Indefinite ‘nil by mouth’ status without other nourishment will end in certain death. This path contrasts with known risks of inhalation pneumonia which arise from eating when the swallowing mechanism is reduced. In a palliative care context, where such a patient may be hungry, careful allied health support may enable the intake of food for comfort and some nourishment.
Famous Quotes
Pope Benedict XVI, in his Angelus address, 2009 stated that “…euthanasia is a false solution to the drama of suffering, a solution unworthy of man. Indeed, the true response cannot be to put someone to death, however ‘kindly’, but rather to witness to the love that helps people to face their pain and agony in a human way. We can be certain that no tear, neither of those who are suffering nor of those who are close to them, is lost before God.”
Legislation in your State/Territory
Australia’s pro-Euthanasia public figure, Philip Nitschke, founder and Director of EXIT International led the charge to pass right to die legislation in the Northern Territory on 25 May 1995. The Rights of the Terminally Ill Act lasted only nine months when it was revoked by the Australian Federal Parliament in 1997, but not before four people were euthanised.
As it stands today, euthanasia laws have been passed in Victoria, Western Australia, Tasmania, South Australia, Queensland and New South Wales.
The Voluntary Assisted Dying Act 2017 came into effect on 19 June 2019 in Victoria while the Voluntary Assisted Dying Act 2019 came into effect in Western Australia on 1 July 2021.
Euthanasia laws will come into effect in Tasmania from 23 October 2022, from 1 January 2023 in Queensland, and from early 2023 in South Australia.
NSW became the last state to legalise euthanasia on May 19, 2022, with 23 votes in favour and 15 against. The laws to come into effect within the next 18 months.
Read your state’s legislation
Victoria: https://www.legislation.vic.gov.au/in-force/acts/voluntary-assisted-dying-act-2017/005
Western Australia: https://www.legislation.wa.gov.au/legislation/prod/filestore.nsf/FileURL/mrdoc_42491.pdf/$FILE/Voluntary%20Assisted%20Dying%20Act%202019%20-%20%5B00-00-00%5D.pdf?OpenElement
Tasmania: https://www.health.tas.gov.au/health-topics/voluntary-assisted-dying
Queensland: https://www.health.qld.gov.au/system-governance/legislation/voluntary-assisted-dying-act
South Australia: https://www.legislation.sa.gov.au/lz?path=%2FC%2FA%2FVOLUNTARY%20ASSISTED%20DYING%20ACT%202021
New South Wales: https://www.parliament.nsw.gov.au/bills/Pages/bill-details.aspx?pk=3891
Voluntary Assisted Dying: Putting Lipstick on a Pig
It should be noted that the laws which have been passed by the various states to legalise assisted suicide all refer to the practice as “voluntary assisted dying”.
However, as Dr John Obeid FRACP Consultant Geriatrician writes in this excellent article; referring to assisted suicide as “voluntary assisted dying” in an attempt to cover up its true nature is like putting lipstick on a pig.
“…putting lipstick on a pig still makes it a pig. Dressing up euthanasia and assisted suicide as “voluntary assisted dying” still tells some people that their life is not worth living, that we have no need or want for them and that they may as well terminate their life…”
Quick Facts
- First Euthanasia Society
- The Hippocratic Corpus
- A Real Fear in Holland
- Euthanasia in Australia
- Euthanasia in Belgium
In 1935, Dr. Killick Millard founded the first euthanasia society in the world, the Voluntary Euthanasia Society in London. The Society is now known as Dignity in Dying. Dr. Millard supported abortion and was a known eugenicist.
Primum non nocere = First do no harm. This edict has been part of medical ethics since the time of the ancient Greek physician, Hippocrates, in the fifth century B.C. It is found in the Hippocratic Corpus, a collection of medical writing attributed to Hippocrates. The original Hippocratic Oath includes: I will apply dietetic measures for the benefit of the sick according to my ability and judgment; I will keep them from harm and injustice.
Euthanasia has been known to be regularly practised in the Netherlands since 1973. Guidelines under Article 293 of the penal code require that a patient’s decision is voluntary, well-considered and persistent, in the presence of unbearable pain without hope of improvement. The decision should be made by more than one doctor, and the doctor and patient should agree that euthanasia is the only reasonable option. However, over the years, much evidence has accumulated to show that these guidelines are commonly disregarded in part or in whole, and that some of them cannot underpin a consistent legal interpretation.
In a growing number of cases, the courts have watered down the interpretation of the law to the point where no physical suffering, indeed no physical illness at all, was required. A case was reported in 2000 where a doctor assisted in the suicide of an 86 year old man, simply because his life had become meaningless. He was later charged with murder, but given a token penalty. Additionally, under-reporting and life-taking without patient request have become common practice for many years.
Medical life-taking without patient consent is also common. In two test cases in different courts in 1995, doctors were exonerated after taking the lives of deformed new-borns, though such victims were of course incapable of consent. Alarmingly, the number of assisted suicides in the Netherlands rose by 13% in 2012.
lifesitenews article from 2022
Report on increased rate of euthanasia after around 20 years in the Netherlands.
Australia’s pro-Euthanasia public figure, Philip Nitschke, founder and Director of EXIT International led the charge to pass right to die legislation in the Northern Territory on 25 May 1995. The Rights of the Terminally Ill Act lasted only nine months when it was revoked by the Australian Federal Parliament in 1997, but not before four people were euthanised.
As it stands today, euthanasia laws have been passed in Victoria, Western Australia, Tasmania, South Australia, Queensland and New South Wales.
The Voluntary Assisted Dying Act 2017 came into effect on 19 June 2019 in Victoria while the Voluntary Assisted Dying Act 2019 came into effect in Western Australia on 1 July 2021.
Euthanasia laws will come into effect in Tasmania from 23 October 2022, from 1 January 2023 in Queensland, and from early 2023 in South Australia.
NSW became the last state to legalise euthanasia on May 19, 2022, with 23 votes in favour and 15 against. The laws to come into effect within the next 18 months.
Read your state’s legislation
Victoria: https://www.legislation.vic.gov.au/in-force/acts/voluntary-assisted-dying-act-2017/005
Western Australia: https://www.legislation.wa.gov.au/legislation/prod/filestore.nsf/FileURL/mrdoc_42491.pdf/$FILE/Voluntary%20Assisted%20Dying%20Act%202019%20-%20%5B00-00-00%5D.pdf?OpenElement
Tasmania: https://www.health.tas.gov.au/health-topics/voluntary-assisted-dying
Queensland: https://www.health.qld.gov.au/system-governance/legislation/voluntary-assisted-dying-act
South Australia: https://www.legislation.sa.gov.au/lz?path=%2FC%2FA%2FVOLUNTARY%20ASSISTED%20DYING%20ACT%202021
New South Wales: https://www.parliament.nsw.gov.au/bills/Pages/bill-details.aspx?pk=3891
Voluntary Assisted Dying: Putting Lipstick on a Pig
It should be noted that the laws which have been passed by the various states to legalise assisted suicide all refer to the practice as “voluntary assisted dying”.
However, as Dr John Obeid FRACP Consultant Geriatrician writes in this excellent article; referring to assisted suicide as “voluntary assisted dying” in an attempt to cover up its true nature is like putting lipstick on a pig.
“…putting lipstick on a pig still makes it a pig. Dressing up euthanasia and assisted suicide as “voluntary assisted dying” still tells some people that their life is not worth living, that we have no need or want for them and that they may as well terminate their life…”
On 13 February 2014, the Belgium Parliament passed a law to extend euthanasia to children. Doctors are now permitted to kill children “under the age of 18” who are terminally ill and suffer from severe pain without any prospect of relief. Read the sad news here: http://www.bbc.co.uk/news/world-europe-26181615
Belgian pediatricians said that the law is not medically necessary as “palliative care teams for children are perfectly capable of achieving pain relief, both in hospital and at home”.

Suggested articles for further reading and links
- B.J. Pollard. The Challenge of Euthanasia. Crows Nest NSW: Little Hills Press Pty Ltd, 1994.
- H.P. Dunn, M.D. Ethics for Doctors, Nurses and Patients. New York: Alba House, 1994.
- HOPE, founder Paul Russell http://noeuthanasia.org.au/
- Euthanasia is out of control in the Netherlands Click Here








